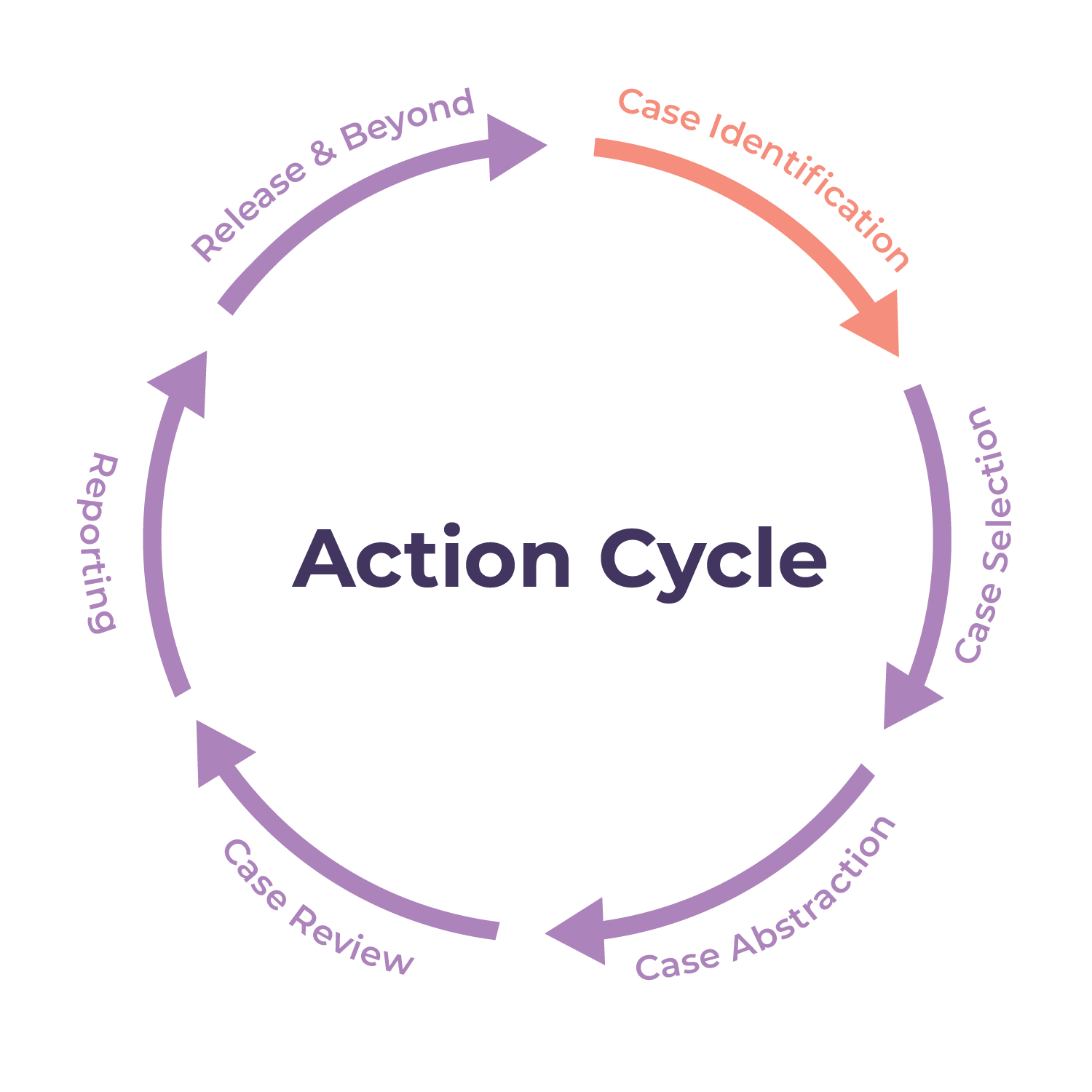
The first task facing a MMRC is the comprehensive identification of pregnancy-associated deaths.
A pregnancy-associated death is the death of a woman while pregnant or within one year of pregnancy, regardless of the cause. For an MMRC to identify all pregnancy-associated deaths, it works with its Office of Vital Records (the official name of this office varies by state). Vital records (birth and death certificates) are the primary sources used for identifying pregnancy-associated deaths. Because no individual method can identify all possible pregnancy-associated deaths in a jurisdiction, MMRCs should use multiple methods to identify these deaths. To adhere to best practices, MMRCs should follow the Reference Guide for Pregnancy-Associated Death Identification.
The Office of Vital Records identifies cases using birth and death certificates in the following ways:
-
Computerized linkages of vital records:
Vital records offices and maternal and child health epidemiologists can link death certificates of reproductive-aged women with other vital records, such as birth certificates and fetal death certificates. These records are linked by common information that is found on both the death certificate of the woman and an infant birth certificate or fetal death certificate, using either deterministic or probabilistic linkage.
-
Pregnancy checkboxes on death certificates:
In 2003, the CDC National Center for Health Statistics released revised standards for live birth, death, and fetal death certificates. The revision of the standard death certificate includes a set of pregnancy-status checkboxes with five options: Not pregnant within the past year, pregnant at time of death, not pregnant but pregnant within 42 days of death, not pregnant but pregnant between 43 days and one year before death, and unknown. Vital records offices use the options selected by death registrars on death certificates to determine if a death meets the definition of pregnancy-associated death. Some jurisdictions have reported inaccurate use of the pregnancy checkboxes among death registrars, therefore MMRCs should not use the checkbox on the death certificate to identify pregnancy-associated deaths without an additional confirmatory source.
-
Direct report from hospitals, providers, medical examiners, and coroners:
Based on legislation or statutory authority, some MMRCs have relationships with hospitals and medical providers to support mandatory or voluntary reporting of deaths in maternity units. Additionally, MMRCs may have relationships with professionals responsible for investigating and certifying deaths (e.g. medical examiners, the state Medical Examiner’s Office, coroners, etc.). These relationships facilitate direct reporting to the MMRC when those professionals receive cases of pregnant women or women who were pregnant within the past year.
-
Publicly Available Online Sources:
MMRC staff with responsibility for identifying maternal deaths may be able to find information about cases through online searches of different outlets, including obituaries, news reports, or social media. For some, these cases may not have been identified by the Office of Vital Records. For example, if the person very recently became pregnant, only close acquaintances may have known.
Identification of Pregnancy-Associated Deaths with a History of SARS-CoV-2 Infection
To improve identification of pregnancy associated deaths with a history of COVID-19, CDC collaborated with 9 jurisdictional health departments to develop best practices for MMRCs. Suggested methods for systematic investigation include the following:
-
Linkages of death records with or manually searching jurisdictional COVID-19 case surveillance databases for pregnancy-associated deaths;
-
Searching cause of death fields on the death record for key terms related to SARS-CoV-2 infection or COVID-19 illness; and
-
Linkages of death records with or manually searching hospital discharge data or other administrative datasets for pregnancy-associated deaths, to ascertain records where there were key terms related to SARS-CoV-2 infection or COVID-19 illness.
CDC is continuing to work with MMRCs to develop best practices for data abstraction and reviews of pregnancy-associated deaths with a history of SARS-CoV-2 infection. Refer to the Identification of Pregnancy-Associated Deaths with a History of SARS-CoV-2 Infection guidance for more information.